Publications 2023
Disrupting Kaposi’s Sarcoma-Associated Herpesvirus (KSHV) Latent Replication with a Small Molecule Inhibitor. Berwanger A, Stein SC, Kany AM, Gartner M, Loretz B, Lehr CM, Hirsch AKH, Schulz TF, Empting M. J Med Chem. 2023 Aug 10;66(15):10782-10790.
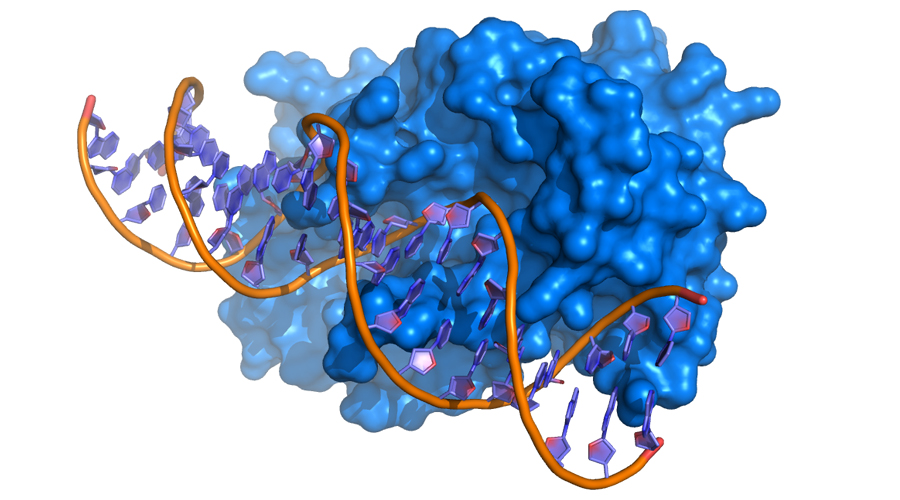
Kaposi sarcoma-associated herpesvirus latency-associated nuclear antigen: more than a key mediator of viral persistence. Schulz TF, Freise A, Stein SC. Curr Opin Virol. 2023 Aug;61:101336. doi: 10.1016/j.coviro.2023.101336. Epub 2023 Jun 16. PMID: 37331160.
The role of nuclear pores and importins for herpes simplex virus infection. Döhner K, Serrero MC, Sodeik B. Curr Opin Virol. 2023 Oct;62:101361. doi: 10.1016/j.coviro.2023.101361. Epub 2023 Sep 4. PMID: 37672874.
Publications 2022
pUL36 Deubiquitinase Activity Augments Both the Initiation and the Progression of Lytic Herpes Simplex Virus Infection in IFN-Primed Cells. Mohnke J, Stark I, Fischer M, Fischer PM, Schlosser A, Grothey A, O’Hare P, Sodeik B, Erhard F, Dölken L, Hennig T. J Virol. 2022 Nov 23;96(22):e0096322. doi: 10.1128/jvi.00963-22. Epub 2022 Oct 31. PMID: 36314822; PMCID: PMC9683058.
Publications 2021
The journey of herpesvirus capsids and genomes to the host cell nucleus. Döhner K, Cornelius A, Serrero MC, Sodeik B. Curr Opin Virol. 2021 Oct;50:147-158. doi: 10.1016/j.coviro.2021.08.005. Epub 2021 Aug 28. PMID: 34464845.
Recent Advances in Developing Treatments of Kaposi’s Sarcoma Herpesvirus-Related Diseases. Naimo E, Zischke J, Schulz TF. Viruses. 2021 Sep 9;13(9):1797. doi: 10.3390/v13091797. PMID: 34578378; PMCID: PMC8473310.
Recruitment of phospholipase Cγ1 to the non-structural membrane protein pK15 of Kaposi Sarcoma-associated herpesvirus promotes its Src-dependent phosphorylation. Samarina N, Ssebyatika G, Tikla T, Waldmann JY, Abere B, Nanna V, Marasco M, Carlomagno T, Krey T, Schulz TF. PLoS Pathog. 2021 Jun 18;17(6):e1009635. doi: 10.1371/journal.ppat.1009635. eCollection 2021 Jun. PMID: 34143834 Free PMC article.
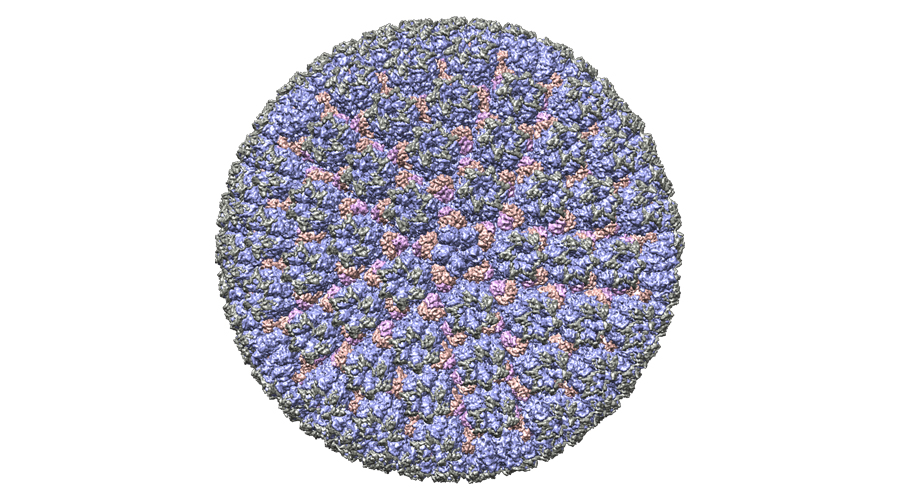
Assembly of infectious Kaposi’s sarcoma-associated herpesvirus progeny requires formation of a pORF19 pentamer. Naniima P, Naimo E, Koch S, Curth U, Alkharsah KR, Ströh LJ, Binz A, Beneke JM, Vollmer B, Böning H, Borst EM, Desai P, Bohne J, Messerle M, Bauerfeind R, Legrand P, Sodeik B, Schulz TF, Krey T. PLoS Biol. 2021 Nov 4;19(11):e3001423.
Interdependent Impact of Lipoprotein Receptors and Lipid-Lowering Drugs on HCV Infectivity. Zapatero-Belinchón, F.J.; Ötjengerdes, R.; Sheldon, J.; Schulte, B.; Carriquí-Madroñal, B.; Brogden, G.; Arroyo-Fernández, L.M.; Vondran, F.W.R.; Maasoumy, B.; von Hahn, T.; Gerold, G. Cells 2021, 10, 1626.
3D culture conditions support Kaposi’s sarcoma herpesvirus (KSHV) maintenance and viral spread in endothelial cells. Dubich T, Dittrich A, Bousset K, Geffers R, Büsche G, Köster M, Hauser H, Schulz TF, Wirth D. J Mol Med (Berl). 2021 Mar;99(3):425-438. doi: 10.1007/s00109-020-02020-8. Epub 2021 Jan 23. PMID: 33484281 Free PMC article.
DNA origami signposts for identifying proteins on cell membranes by electron cryotomography. Silvester E, Vollmer B, Pražák V, Vasishtan D, Machala EA, Whittle C, Black S, Bath J, Turberfield AJ, Grünewald K, Baker LA. Cell. 2021 Feb 18;184(4):1110-1121.e16. doi: 10.1016/j.cell.2021.01.033. PMID: 33606980; PMCID: PMC7895908.
Phenotypical Characterization of the Nuclear Egress of Recombinant Cytomegaloviruses Reveals Defective Replication upon ORF-UL50 Deletion but Not pUL50 Phosphosite Mutation. Häge S, Sonntag E, Svrlanska A, Borst EM, Stilp AC, Horsch D, Müller R, Kropff B, Milbradt J, Stamminger T, Schlötzer-Schrehardt U, Marschall M. Viruses. 2021 Jan 22;13(2):165. doi: 10.3390/v13020165. PMID: 33499341; PMCID: PMC7911381.
The Complex Regulatory Role of Cytomegalovirus Nuclear Egress Protein pUL50 in the Production of Infectious Virus. Häge S, Büscher N, Pakulska V, Hahn F, Adrait A, Krauter S, Borst EM, Schlötzer-Schrehardt U, Couté Y, Plachter B, Marschall M. Cells. 2021 Nov 11;10(11):3119. doi: 10.3390/cells10113119. PMID: 34831342; PMCID: PMC8625744.
Freiburg index of post-TIPS survival (FIPS) a valid prognostic score in patients with cirrhosis but also an advisor against TIPS? Stockhoff L, Schneider H, Tergast TL, Cornberg M, Maasoumy B. J Hepatol. 2021 Aug;75(2):487-489. doi: 10.1016/j.jhep.2021.02.031. Epub 2021 Mar 12. PMID: 33716088.
IgG, a novel predictor for acute-on-chronic liver failure and survival in patients with decompensated cirrhosis? Tergast TL, Schultalbers M, Wedemeyer H, Cornberg M, Maasoumy B. J Hepatol. 2021 Jul;75(1):229-231. doi: 10.1016/j.jhep.2021.01.040. Epub 2021 Feb 4. PMID: 33548386.
Publications 2020
Targeting Kaposi’s Sarcoma-Associated Herpesvirus ORF21 Tyrosine Kinase and Viral Lytic Reactivation by Tyrosine Kinase Inhibitors Approved for Clinical Use. J Virol. Beauclair G, Naimo E, Dubich T, Rückert J, Koch S, Dhingra A, Wirth D, Schulz TF. 2020 Feb 14;94(5):e01791-19. doi: 10.1128/JVI.01791-19. PMID: 31826996; PMCID: PMC7022342.
Acid ceramidase of macrophages traps herpes simplex virus in multivesicular bodies and protects from severe disease. Lang J, Bohn P, Bhat H, Jastrow H, Walkenfort B, Cansiz F, Fink J, Bauer M, Olszewski D, Ramos-Nascimento A, Duhan V, Friedrich SK, Becker KA, Krawczyk A, Edwards MJ, Burchert A, Huber M, Friebus-Kardash J, Göthert JR, Hardt C, Probst HC, Schumacher F, Köhrer K, Kleuser B, Babiychuk EB, Sodeik B, Seibel J, Greber UF, Lang PA, Gulbins E, Lang KS. Nat Commun. 2020 Mar 12;11(1):1338. doi: 10.1038/s41467-020-15072-8. PMID: 32165633; PMCID: PMC7067866.
Quantitative Proteomics Analysis of Lytic KSHV Infection in Human Endothelial Cells Reveals Targets of Viral Immune Modulation Gabaev I, Williamson JC, Crozier TWM, Schulz TF, Lehner PJ. Cell Rep 2020;33(2):108249
Discovery of Novel Latency-Associated Nuclear Antigen Inhibitors as Antiviral Agents Against Kaposi’s Sarcoma-Associated Herpesvirus ACS Kirsch P, Jakob V, Elgaher WAM, Walt C, Oberhausen K, Schulz TF, Empting M. Chem Biol 2020;15(2):388-395
Hit-to-lead optimization of a latency-associated nuclear antigen inhibitor against Kaposi’s sarcoma-associated herpesvirus infections Kirsch P, Stein SC, Berwanger A, Rinkes J, Jakob V, Schulz TF, Empting M. Eur J Med Chem 2020;202:112525
Brd/BET Proteins Influence the Genome-Wide Localization of the Kaposi’s Sarcoma-Associated Herpesvirus and Murine Gammaherpesvirus Major Latency Proteins Lotke R, Schneeweiss U, Pietrek M, Günther T, Grundhoff A, Weidner-Glunde M, Schulz TF. Front Microbiol 2020;11:591778
Whole-Genome Approach to Assessing Human Cytomegalovirus Dynamics in Transplant Patients Undergoing Antiviral Therapy Suarez NM, Blyth E, Li K, Ganzenmueller T, Camiolo S, Avdic S, Withers B, Linnenweber-Held S, Gwinner W, Dhingra A, Heim A, Schulz TF, Gunson R, Gottlieb D, Slobedman B, Davison AJ. Front Cell Infect Microbiol 2020;10:267
Cellular Electron Cryo-Tomography to Study Virus-Host Interactions. Quemin ERJ, Machala EA, Vollmer B, Pražák V, Vasishtan D, Rosch R, Grange M, Franken LE, Baker LA, Grünewald K. Annu Rev Virol. 2020 Sep 29;7(1):239-262. doi: 10.1146/annurev-virology-021920-115935. Epub 2020 Jul 6. PMID: 32631159.
The Proteome and Secretome of Cortical Brain Cells Infected With Herpes Simplex Virus Front. Niko Hensel, Verena Raker, Benjamin Förthmann, Anna Buch, Beate Sodeik, Andreas Pich, Peter Claus, Neurol., 27 August 2020, Sec. Neuroinfectious Diseases, Volume 11 – 2020, https://doi.org/10.3389/fneur.2020.00844
Publications 2019
Fragment-Based Discovery of a Qualified Hit Targeting the Latency-Associated Nuclear Antigen of the Oncogenic Kaposi’s Sarcoma-Associated Herpesvirus/Human Herpesvirus 8. Kirsch P, Jakob V, Oberhausen K, Stein SC, Cucarro I, Schulz TF, Empting M. J Med Chem. 2019 Apr 25;62(8):3924-3939. doi: 10.1021/acs.jmedchem.8b01827. Epub 2019 Apr 12. PMID: 30888817.
Kaposi’s sarcoma-associated herpesvirus vIRF2 protein utilizes an IFN-dependent pathway to regulate viral early gene expression Koch S, Damas M, Freise A, Hage E, Dhingra A, Rückert J, Gallo A, Kremmer E, Tegge W, Brönstrup M, Brune W, Schulz TF. PLoS Pathog 2019;15(5):e1007743 D1
Autophagic degradation of lamins facilitates the nuclear egress of herpes simplex virus type 1. Turan A, Grosche L, Krawczyk A, Mühl-Zürbes P, Drassner C, Düthorn A, Kummer M, Hasenberg M, Voortmann S, Jastrow H, Dörrie J, Schaft N, Kraner M, Döhner K, Sodeik B, Steinkasserer A, Heilingloh CS. J Cell Biol. 2019 Feb 4;218(2):508-523. doi: 10.1083/jcb.201801151. Epub 2018 Dec 26. PMID: 30587512; PMCID: PMC6363456.
Fragment-Based Discovery of a Qualified Hit Targeting the Latency-Associated Nuclear Antigen of the Oncogenic Kaposi’s Sarcoma-Associated Herpesvirus/Human Herpesvirus 8 Philine Kirsch, Valentin Jakob, +4 authors M. Empting. Journal of Medicinal Chemistry. 19 March 2019 DOI:10.1021/acs.jmedchem.8b01827Corpus ID: 84183173