Publications 2023
An expanded CRISPR-Cas9-assisted recombineering toolkit for engineering genetically intractable Pseudomonas aeruginosa isolates. Pankratz D, Gomez NO, Nielsen A, Mustafayeva A, Gür M, Arce-Rodriguez F, Nikel PI, Häussler S, Arce-Rodriguez A. Nat Protoc. 2023 Nov;18(11):3253-3288.
Transcriptome Dynamics of Pseudomonas aeruginosa during Transition from Overlapping To Non-Overlapping Cell Cycles. Alpers K, Vatareck E, Gröbe L, Müsken M, Scharfe M, Häussler S, Tomasch J. mSystems. 2023 Feb 14:e0113022.
The Origin of the Intracellular Silver in Bacteria: A Comprehensive Study using Targeting Gold-Silver Alloy Nanoparticles. Streich C, Stein F, Jakobi J, Ingendoh-Tsakmakidis A, Heine N, Rehbock C, Winkel A, Grade S, Kühnel M, Migunov V, Kovács A, Knura T, Stiesch M, Sures B, Barcikowski S. Adv Healthc Mater. 2023 Dec;12(30):e2302084. doi: 10.1002/adhm.202302084. Epub 2023 Sep 17. PMID: 37661312.
Publications 2022
Distinct Long- and Short-Term Adaptive Mechanisms in Pseudomonas aeruginosa. Koska M, Kordes A, Erdmann J, Willger SD, Thöming JG, Bähre H, Häussler S. Microbiol Spectr. 2022 Dec 21;10(6):e0304322. Epub 2022 Nov 14.
Genomic epidemiology of clinical ESBL-producing Enterobacteriaceae in a German hospital suggests infections are primarily community- and regionally-acquired. Neffe L, Forde TL, Oravcova K, Köhler U, Bautsch W, Tomasch J, Häussler S. Microb Genom. 2022 Dec;8(12):mgen000901.
Transcriptional Profiling of Pseudomonas aeruginosa Infections. Thöming JG, Häussler S. Adv Exp Med Biol. 2022;1386:303-323.
Evolution of biofilm-adapted gene expression profiles in lasR-deficient clinical Pseudomonas aeruginosa isolates. Jeske A, Arce-Rodriguez A, Thöming JG, Tomasch J, Häussler S. NPJ Biofilms Microbiomes.
Pseudomonas aeruginosa Is More Tolerant Under Biofilm Than Under Planktonic Growth Conditions: A Multi-Isolate Survey. Thöming JG, Häussler S. Front Cell Infect Microbiol.
Pseudomonas aeruginosa post-translational responses to elevated c-di-GMP levels. Bense S, Witte J, Preuße M, Koska M, Pezoldt L, Dröge A, Hartmann O, Müsken M, Schulze J, Fiebig T, Bähre H, Felgner S, Pich A, Häussler S. Mol Microbiol.
Critical Assessment of Metagenome Interpretation: the second round of challenges. Meyer F, Fritz A, Deng ZL, Koslicki D, Lesker TR, Gurevich A, Robertson G, Alser M, Antipov D, Beghini F, Bertrand D, Brito JJ, Brown CT, Buchmann J, Buluç A, Chen B, Chikhi R, Clausen PTLC, Cristian A, Dabrowski PW, Darling AE, Egan R, Eskin E, Georganas E, Goltsman E, Gray MA, Hansen LH, Hofmeyr S, Huang P, Irber L, Jia H, Jørgensen TS, Kieser SD, Klemetsen T, Kola A, Kolmogorov M, Korobeynikov A, Kwan J, LaPierre N, Lemaitre C, Li C, Limasset A, Malcher-Miranda F, Mangul S, Marcelino VR, Marchet C, Marijon P, Meleshko D, Mende DR, Milanese A, Nagarajan N, Nissen J, Nurk S, Oliker L, Paoli L, Peterlongo P, Piro VC, Porter JS, Rasmussen S, Rees ER, Reinert K, Renard B, Robertsen EM, Rosen GL, Ruscheweyh HJ, Sarwal V, Segata N, Seiler E, Shi L, Sun F, Sunagawa S, Sørensen SJ, Thomas A, Tong C, Trajkovski M, Tremblay J, Uritskiy G, Vicedomini R, Wang Z, Wang Z, Wang Z, Warren A, Willassen NP, Yelick K, You R, Zeller G, Zhao Z, Zhu S, Zhu J, Garrido-Oter R, Gastmeier P, Hacquard S, Häußler S, Khaledi A, Maechler F, Mesny F, Radutoiu S, Schulze-Lefert P, Smit N, Strowig T, Bremges A, Sczyrba A, McHardy AC. Nat Methods.
Rapid and accurate identification of ribosomal RNA sequences via deep learning. Deng ZL, Münch PC, Mreches R, McHardy AC. Nucleic Acids Res.
Publications 2021
Quo vadis clinical diagnostic microbiology? Haag S, Häussler S. Clin Microbiol Infect.
Removable denture is a risk indicator for peri-implantitis and facilitates expansion of specific periodontopathogens: a cross-sectional study. Grischke J, Szafrański SP, Muthukumarasamy U, Haeussler S, Stiesch M. BMC Oral Health.
Publications 2020
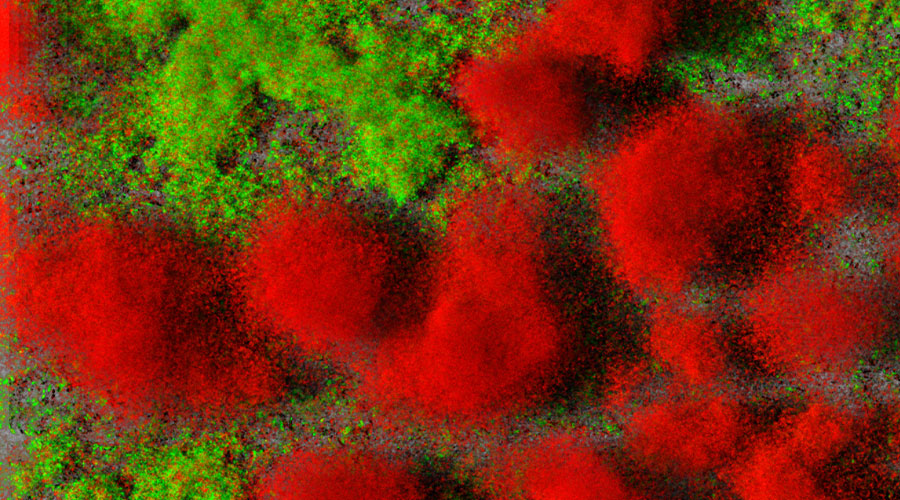
Parallel evolutionary paths to produce more than one Pseudomonas aeruginosa biofilm phenotype. Thöming JG, Tomasch J, Preusse M, Koska M, Grahl N, Pohl S, Willger SD, Kaever V, Müsken M, Häussler S. NPJ Biofilms Microbiomes.
Genetic determinants of Pseudomonas aeruginosa fitness during biofilm growth. Schinner S, Engelhardt F, Preusse M, Thöming JG, Tomasch J, Häussler S. Biofilm.
Organism-specific depletion of highly abundant RNA species from bacterial total RNA. Engelhardt F, Tomasch J, Häussler S. Access Microbiol.
Host-induced spermidine production in motile Pseudomonas aeruginosa triggers phagocytic uptake. Felgner S, Preusse M, Beutling U, Stahnke S, Pawar V, Rohde M, Brönstrup M, Stradal T, Häussler S. Elife.
Analysis of the organization and expression patterns of the convergent Pseudomonas aeruginosa lasR/rsaL gene pair uncovers mutual influence. Schinner S, Preusse M, Kesthely C, Häussler S. Mol Microbiol.
Targeting bioenergetics is key to counteracting the drug-tolerant state of biofilm-grown bacteria. Donnert M, Elsheikh S, Arce-Rodriguez A, Pawar V, Braubach P, Jonigk D, Haverich A, Weiss S, Müsken M, Häussler S.PLoS Pathog.
Evolution of Pseudomonas aeruginosa toward higher fitness under standard laboratory conditions. Grekov I, Thöming JG, Kordes A, Häussler S. ISME J.
Expression of the MexXY Aminoglycoside Efflux Pump and Presence of an Aminoglycoside-Modifying Enzyme in Clinical Pseudomonas aeruginosa Isolates Are Highly Correlated. Seupt A, Schniederjans M, Tomasch J, Häussler S. Antimicrob Agents Chemother.
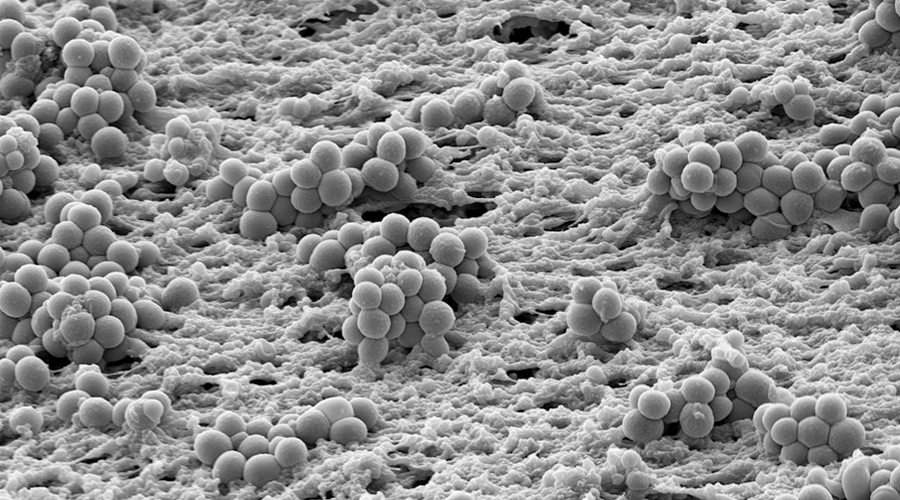
Biofilm formation on zirconia and titanium over time-An in vivo model study. Desch A, Freifrau von Maltzahn N, Stumpp N, Dalton M, Yang I, Stiesch M. Clin Oral Implants Res. 2020 Sep;31(9):865-880. doi: 10.1111/clr.13632. Epub 2020 Jul 9. PMID: 32583509.
Non-Invasive Luciferase Imaging of Type I Interferon Induction in a Transgenic Mouse Model of Biomaterial Associated Bacterial Infections: Microbial Specificity and Inter-Bacterial Species Interactions. Rahim MI, Winkel A, Lienenklaus S, Stumpp NS, Szafrański SP, Kommerein N, Willbold E, Reifenrath J, Mueller PP, Eisenburger M, Stiesch M. Microorganisms. 2020 Oct 21;8(10):1624. doi: 10.3390/microorganisms8101624. PMID: 33096869; PMCID: PMC7589032.
Predicting antimicrobial resistance in Pseudomonas aeruginosa with machine learning-enabled molecular diagnostics. Khaledi A, Weimann A, Schniederjans M, Asgari E, Kuo TH, Oliver A, Cabot G, Kola A, Gastmeier P, Hogardt M, Jonas D, Mofrad MR, Bremges A, McHardy AC, Häussler S. EMBO Mol Med. 2020 Mar 6;12(3):e10264. doi: 10.15252/emmm.201910264. Epub 2020 Feb 12. PMID: 32048461; PMCID: PMC7059009.
Publications 2019
Establishment of an induced memory response in Pseudomonas aeruginosa during infection of a eukaryotic host. Kordes A, Grahl N, Koska M, Preusse M, Arce-Rodriguez A, Abraham WR, Kaever V, Häussler S. ISME J.
Genetically diverse Pseudomonas aeruginosa populations display similar transcriptomic profiles in a cystic fibrosis explanted lung. Kordes A, Preusse M, Willger SD, Braubach P, Jonigk D, Haverich A, Warnecke G, Häussler S. Nat Commun.
The CAFA challenge reports improved protein function prediction and new functional annotations for hundreds of genes through experimental screens. Zhou N, Jiang Y, Bergquist TR, Lee AJ, Kacsoh BZ, Crocker AW, Lewis KA, Georghiou G, Nguyen HN, Hamid MN, Davis L, Dogan T, Atalay V, Rifaioglu AS, Dalkıran A, Cetin Atalay R, Zhang C, Hurto RL, Freddolino PL, Zhang Y, Bhat P, Supek F, Fernández JM, Gemovic B, Perovic VR, Davidović RS, Sumonja N, Veljkovic N, Asgari E, Mofrad MRK, Profiti G, Savojardo C, Martelli PL, Casadio R, Boecker F, Schoof H, Kahanda I, Thurlby N, McHardy AC, Renaux A, Saidi R, Gough J, Freitas AA, Antczak M, Fabris F, Wass MN, Hou J, Cheng J, Wang Z, Romero AE, Paccanaro A, Yang H, Goldberg T, Zhao C, Holm L, Törönen P, Medlar AJ, Zosa E, Borukhov I, Novikov I, Wilkins A, Lichtarge O, Chi PH, Tseng WC, Linial M, Rose PW, Dessimoz C, Vidulin V, Dzeroski S, Sillitoe I, Das S, Lees JG, Jones DT, Wan C, Cozzetto D, Fa R, Torres M, Warwick Vesztrocy A, Rodriguez JM, Tress ML, Frasca M, Notaro M, Grossi G, Petrini A, Re M, Valentini G, Mesiti M, Roche DB, Reeb J, Ritchie DW, Aridhi S, Alborzi SZ, Devignes MD, Koo DCE, Bonneau R, Gligorijević V, Barot M, Fang H, Toppo S, Lavezzo E, Falda M, Berselli M, Tosatto SCE, Carraro M, Piovesan D, Ur Rehman H, Mao Q, Zhang S, Vucetic S, Black GS, Jo D, Suh E, Dayton JB, Larsen DJ, Omdahl AR, McGuffin LJ, Brackenridge DA, Babbitt PC, Yunes JM, Fontana P, Zhang F, Zhu S, You R, Zhang Z, Dai S, Yao S, Tian W, Cao R, Chandler C, Amezola M, Johnson D, Chang JM, Liao WH, Liu YW, Pascarelli S, Frank Y, Hoehndorf R, Kulmanov M, Boudellioua I, Politano G, Di Carlo S, Benso A, Hakala K, Ginter F, Mehryary F, Kaewphan S, Björne J, Moen H, Tolvanen MEE, Salakoski T, Kihara D, Jain A, Šmuc T, Altenhoff A, Ben-Hur A, Rost B, Brenner SE, Orengo CA, Jeffery CJ, Bosco G, Hogan DA, Martin MJ, O’Donovan C, Mooney SD, Greene CS, Radivojac P, Friedberg I. Genome Biol. 2019 Nov 19;20(1):244.
Diversity patterns of bacteriophages infecting Aggregatibacter and Haemophilus species across clades and niches. Szafrański SP, Kilian M, Yang I, Bei der Wieden G, Winkel A, Hegermann J, Stiesch M. ISME J.